
ĭespite the importance of recognizing chronic mucosal changes in the biopsies of patients with IBD, it has been well documented that initial colonic or rectal biopsies from 10% to 34% of pediatric patients ultimately shown to have UC lacked architectural distortion or other histologic features of chronic colitis. Multiple biopsy studies of new-onset IBD in adults have shown that histologic features of chronic damage as noted above can reliably distinguish IBD from self-limited colitis. The histologic diagnosis of IBD rests on the recognition of chronic mucosal damage, chronic colitis. Although numerous crypt abscesses suggest UC, they may be noted in CD as well as in infections and Clostridium difficile–related injury.
Neutrophils may also invade the crypt epithelium (cryptitis) or form small abscesses within the crypt lumen (crypt abscesses). Neutrophils in these cases predominate in the superficial portion of the mucosa, and may be associated with small erosions or ulcers. ASLC is characterized by a predominantly neutrophilic infiltrate without significant crypt architectural changes. However, microbiologic investigations can reveal a colitis-causing pathogen such as Salmonella, Campylobacter, and Yersinia in up to 15% of patients with IBD. Stool cultures and duration of diarrhea may help, as patients without an identifiable pathogen or in whom diarrhea lasts more than several weeks are more likely to have IBD. Chronic active colitis refers to the presence of a neutrophilic infiltrate superimposed on the above changes, and is usually seen during exacerbations of IBD.Įndoscopic features alone may not reliably distinguish acute self-limited colitis (ASLC) from IBD. Though considered a hallmark of chronic idiopathic inflammatory bowel disease, histologic features of chronicity may also be seen in other settings in pediatrics, such as immunodeficiency disorders, metabolic diseases such as glycogen storage disease type Ib, or result from mucosal injury due to ischemia or Hirschsprung’s disease. The presence of an increased mononuclear inflammatory cell infiltrate, usually an integral part of the process, is the least useful histologic parameter given the wide range in numbers of lymphocytes and plasma cells in normal specimens. It is more frequently noted in Crohn’s disease than ulcerative colitis (UC), but is also a useful feature of chronic damage. Pyloric metaplasia is the presence of mucous glands normally present in the gastric antrum and pylorus. In the normal colon, Paneth cells usually extend into the right colon, but their presence in the left colon is a feature of chronic damage, especially in the older child.

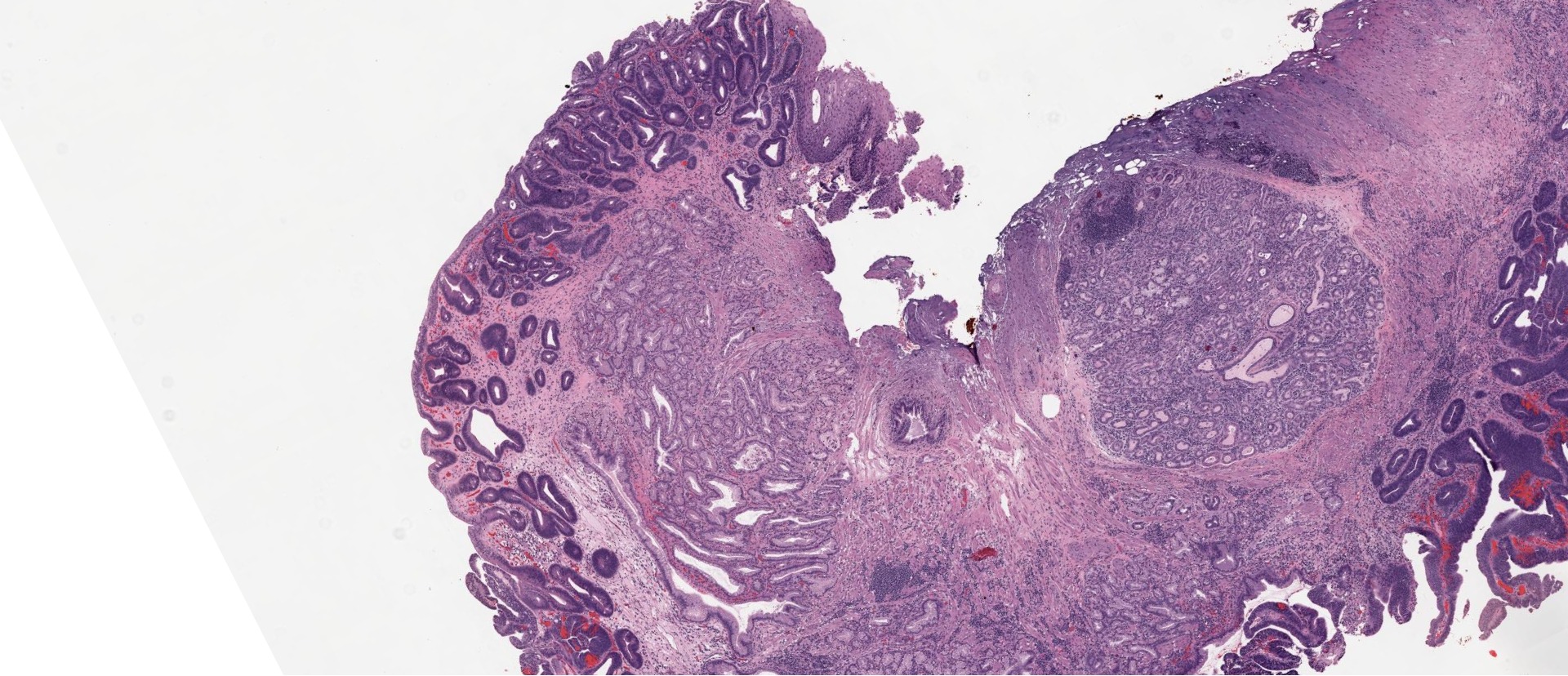
Paneth cell metaplasia and pyloric metaplasia are other useful findings (Fig. Shortening of the crypts is most often due to the presence of a basally situated chronic inflammatory infiltrate (basal plasmacytosis), which separates the base of the crypts from the muscularis mucosae (Fig. The features of chronic colitis are based on the recognition of architectural changes in the mucosa, such as a “villiform” aspect of the surface epithelium, crypt destruction, and atrophy, and shortening of the crypts with irregular branching and loss of their regular outline.


 0 kommentar(er)
0 kommentar(er)
